
Day in the life of an Emergency Medicine ST1
What is being an Emergency Medicine ST1 really like? If you’re considering specialising in Emergency Medicine, or have started preparing your application, hopefully, this blog will give you an insight into what the training is actually like!
Most emergency medicine (EM) trainees will start by completing the ACCS programme (CT/ST1-3) before moving on to higher specialty training (ST4-6). Alternatively, the DRE-EM (Defined Route of Entry into Emergency Medicine) pathway provides ST3 entry for those who have completed approved training in surgery, acute medicine, anaesthetics or intensive care.
The ACCS programme for Emergency Medicine is three years long and can either be run-through or standalone, giving you the choice to guarantee staying in the same deanery for your higher specialty training or have the option to apply elsewhere. During the first two years, trainees rotate between emergency medicine, acute medicine, anaesthetics and intensive care, typically with six months in each. The third year is spent in an emergency department with a large proportion of the time focused on paediatric emergency medicine (PEM).
ST1 Emergency Medicine Rotation
Shifts in emergency departments are variable and will include a range of days, nights and weekends. If starting at a key handover time, I start the shift alongside the whole team as we talk through the list of patients in the department, clarifying plans and which clinician is going to take these forward. We also identify anyone that was particularly unwell or any special circumstances we needed to be aware of such as patients awaiting transfer to a different hospital. This board round is led by a consultant; we’re one of the few specialties where there’s often a consultant present 24/7 (although this varies depending on the hospital), and the whole team of doctors, advanced clinical practitioners and physician associates attend.
After clarifying where the consultants would like me to start (minors, majors, resus or ‘RAP’, the ambulance receiving area), I head to the area, introduce myself to the team and review the list of patients waiting to be seen. If in resus, I’ll receive a handover of all of the patients in there and find out about any imminent arrivals that the ambulance service has phoned through in advance. Sometimes called a ‘pre-alert’ or ‘ASHICE’, this is a way of generating a specific response before the patient arrives, such as gathering a trauma team. Then, I’ll put my name against the next patient to be seen, normally in time order, but by acuity where required, read the triage and ambulance notes, review any relevant previous attendances or other health records if possible, then go and meet the patient.
One of the beautiful things about emergency medicine is its unpredictability. You will see the full spectrum of life, from newborns to centenarians, with all manner of presentations. Some will present with flares of chronic disease, some with traumatic injuries, and others still with acute medical problems. The required knowledge level is broad and deep, but the approach is always similar. You will take a history (from the patient, from relatives, from emergency services present), perform an examination (generally ABCDE to start for anyone in RAP/majors/resus, or a focused exam for minors), arrange and interpret investigations (x-rays, ultrasound, CT scans, bloods, blood gases, urine dips, peak flows etc) and work to establish a diagnosis or exclude significant pathology if a definitive diagnosis is not possible, before starting treatment.
You will have the opportunity to work in and be supported to lead teams working together to resuscitate unstable patients. You will learn and perform procedures including joint and fracture manipulations, cardioversion, nerve blocks and more. In addition, you’ll communicate with different specialties and refer patients where appropriate. All the while, you’ll be supported by a senior team and will be constantly learning.
ST1 Acute Medicine Rotation
The acute medicine rotation is very different to your emergency medicine one. Your focus will narrow, but the length of time you have with each patient and depth of investigation and treatment will increase. Acute medical units tend to be high-throughput areas, trying to turn patients around and discharge them within 48 hours, or admit them to a ward if that’s not possible. You’ll see a range of acute and chronic medical presentations from across the internal medicine spectrum, from rheumatological to respiratory, and endocrine to neurological. If you can’t remember the difference between ANCA and ANA, or really want to develop your understanding of hyponatraemia, this is the placement in which you’ll achieve that!
Ward days typically start with a senior-led ward round, and as an ST1 you’ll generally prepare the notes, recap the story so far, and then scribe during the round. Ward rounds are often followed by board rounds with the multidisciplinary team to ensure shared awareness of medical, nursing, therapy and discharge plans. The rest of the day will involve implementing the medical plans; prescribing what needs to be prescribed, arranging and interpreting appropriate investigations, liaising with specialties and families, and progressing discharge plans. These days are typically 09:00-17:00 or similar.
On-call days are generally split into either clerking or ward cover. These tend to be longer, up to 12.5 hours, during which the clerking doctors will review patients referred for a medical admission from A&E, clinics, or primary care, and prepare them for the consultant post-take ward round. Like in A&E, but with a bit more time and access to more medical investigations, you’ll review the patient, take a history and perform an examination, and try to progress their clinical care. You’ll present the patient to a consultant during the (normally twice-daily) post-take ward rounds and receive feedback on your diagnostic and management skills.
On-call ward cover shifts involve looking after the wards whilst the normal ‘day teams’ aren’t around, completing the tasks handed over either by the ward team, as well as reviewing any sick patients and escalating or palliating where appropriate. These are often very busy shifts so it’s worth wearing your pedometer! You’ll also be part of the resuscitation team, attending medical emergency calls and cardiac arrests. Best practice is for these teams to meet, introduce and allocate roles at the beginning of each shift. As an emergency medicine trainee, you’ll often bring excellent skills to these calls.
Training when completing Emergency Medicine ST1
There’s a mandatory requirement to complete a Kaizen ePortfolio (which will only cost you £322 for 2023-24, as part of your required subscription to the Royal College of Emergency Medicine). You’ll need to demonstrate growth and development via CBDs, DOPS, MiniCEXs and MSFs. There’s a list of procedures that you’ll need to be signed off for during ACCS, from chest drains to external pacing to central lines, with clearly stated ‘entrustment’ levels required for each skill.
You will have access to generous amounts of study leave and study budget with the ability to attend required (ALS, EPALS, ATLS etc), optional (MIMMS, PHEC, EMTA conference etc) and aspirational (DipIMC, cardiac arrest symposium, international conferences) courses, examinations and CPD opportunities. You’ll have an ACCS Lead for your trust as well as appointed Educational and Clinical Supervisors, who are all there to support your development.
Alongside this, you’ll have regional ACCS training days on a monthly basis that cover the curriculum, as well as local teaching on each placement.
There’s also the ability to complete the ACCS programme whilst working less than full time, and to take time out when required. The faculty are supportive and understanding, and they want you to succeed.
The combination of service delivery, on-the-job mentoring and structured courses will hopefully see you flourish as you work towards becoming an emergency medicine maestro. At some point, you’ll even be able to tell your friends that work has appointed you as ‘EPIC’ –whether you tell them that it means ‘emergency physician in charge’ is entirely up to you!
If you have already applied for Emergency Medicine training and you are currently preparing for your MSRA or interview, check out our MSRA Complete Guide 2025, guide to the ACCS Emergency Medicine Interview and our ACCS Emergency Medicine Interview Question bank, providing a comprehensive set of questions and answers to help you prepare for that all important interview.
This blog was written by Luke Tester, an emergency medicine trainee in South East England, and we hope it has given you an insight into what to expect!
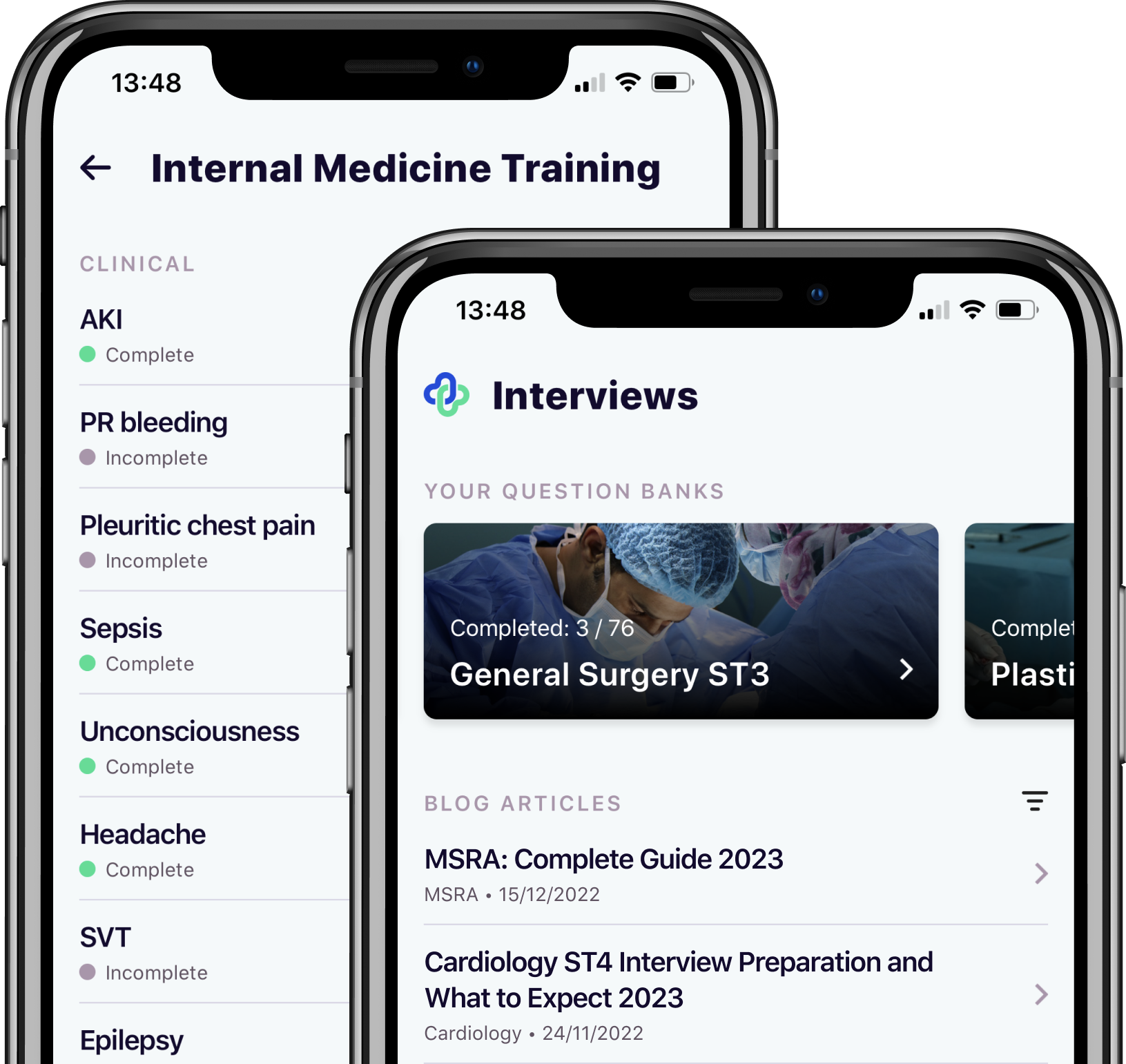
Take your subscriptions with you
Our mobile app allows you to access your interview and exam question banks wherever you are.




