Ophthalmology ST1 Interview: 2024 Guide
If you’re considering applying for Ophthalmology ST1, this guide will provide everything you need to know about the application process, key recruitment dates and the interview format.
Ophthalmology ST1 is a competitive pathway. In 2023, there were 971 applications for just 98 posts, giving a competition ratio of 9.91. This means there were almost 10 applications for every post available. With this kind of competition, it’s essential that you prepare well for the interview and perform to the best of your ability.
Ophthalmology ST1 Key Dates
The 2024 recruitment dates for Ophthalmology ST1 are as follows:
| Stage | Date |
|---|---|
| Applications published | 25 October 2023 |
| Applications open | 26 October 2023 |
| Applications close | 23 November 2023 |
| Longlisting from | 27 November 2023 |
| Invitation to book MSRA expected no later than | 19 December 2023 |
| Multi-Specialty Recruitment Assessment (MSRA) | 4 – 14 January 2024 |
| Documentation upload window | 7 – 13 February 2024 |
| Candidates invited to book an interview slot | 6 March 2024 |
| Preferences open | TBC |
| Interview date | 15 March 2024 |
| Feedback released | 22 March 2024 |
| Offers released by no later than | 26 March 2024 |
Ophthalmology ST1 Application
For 2024, the selection process consists of the following three components, which we will cover in more detail in the sections below:
You must also ensure you meet the essential eligibility criteria outlined in the person specification. There is no shortlisting as part of the Ophthalmology ST1 selection process for 2024; instead, the 300 highest scoring MSRA applicants will be invited for interview.
Following the interview, your performance in the evidence folder and online interview will be combined to give you an overall score, which is used to rank you against other candidates. The maximum score for each component is as follows:
- Evidence Folder – Maximum 50 points
- Online interview – Maximum 50 points
Doing well in the MRSA exam will get you that interview, and then your interview and evidence folder are key to get you that offer; targeting your revision over just a few months will help you achieve highly in the MSRA and interview!
Ophthalmology ST1 Evidence Folder
As mentioned above, you must submit an evidence folder as part of the selection process. This involves uploading documents to a specifically designed online portal to demonstrate your achievements within the set domains; for example, qualifications, prizes/awards and commitment to ophthalmology (e.g. electives/taster weeks). Your evidence folder will be scored against a set criteria for each domain.
For more information and a full breakdown of the evidence folder domains and scoring, please see our 2024 guide to the Ophthalmology ST1 Interview Evidence Folder.
Crucially, your evidence folder should be clearly laid out, following the mark scheme to the letter, as you have no opportunity to explain or present your contents. Therefore, it is vital that it is organised and everything that is worth points is easily navigable and scored for your benefit. Everything that is unnecessary should be left out, as it detracts the interviewers’ attention.
There are a few ways to gain some last-minute marks if you haven’t already got them. For example, you can “design an educational course” via an e-learning tool, which you can put together in your local hospital. Alternatively, you can gain 0.5 points for simply completing a course like the Medibuddy Teach the Teacher course. In “commitment to ophthalmology”, if you haven’t already, you can ask your friendly local ophthalmologist to spend time with them in eye casualty (with a letter as evidence for points). There are also marks for the use of the EyeSi programme, which is a microsurgical simulator that junior trainees use, for example, in training for independent cataract surgery. Only a few units, such as Moorfields Eye Hospital, Western Eye Hospital and the Royal College of Ophthalmologists, have this simulator, and the best way to access these is to ask an ophthalmology trainee.
For more advice on structuring your evidence folder and using what you already have to maximise marks, check out our blog post on preparing your evidence folder.
Teach the Teacher Course by Medibuddy
This two-day CPD-accredited online course will earn you 12 CPD points on completion. It’s entirely flexible, so you can complete it in two days or multiple sessions over a longer period. On completion of the course, you’ll receive a certificate for your portfolio that is accredited for CCT, interviews and appraisals.
Find out moreMulti-specialty Recruitment Assessment (MSRA) Exam
The MSRA is a multiple-choice exam that is also taken by GP, radiology, emergency medicine and other specialty applicants. It consists of an SJT-type component and a general medical questions component.
The best advice for this is to do as much practice as possible. It is not a difficult exam, but you need to do reasonably well to simply get an interview. The cut-off score for interview will vary from year to year.
For 2024, the exam will be held between Thursday 4 January and Sunday 14 January 2024, at Pearson Vue test centres. Most applicants will spend months preparing for this exam, so we recommend you do the same to increase your chances of scoring well.
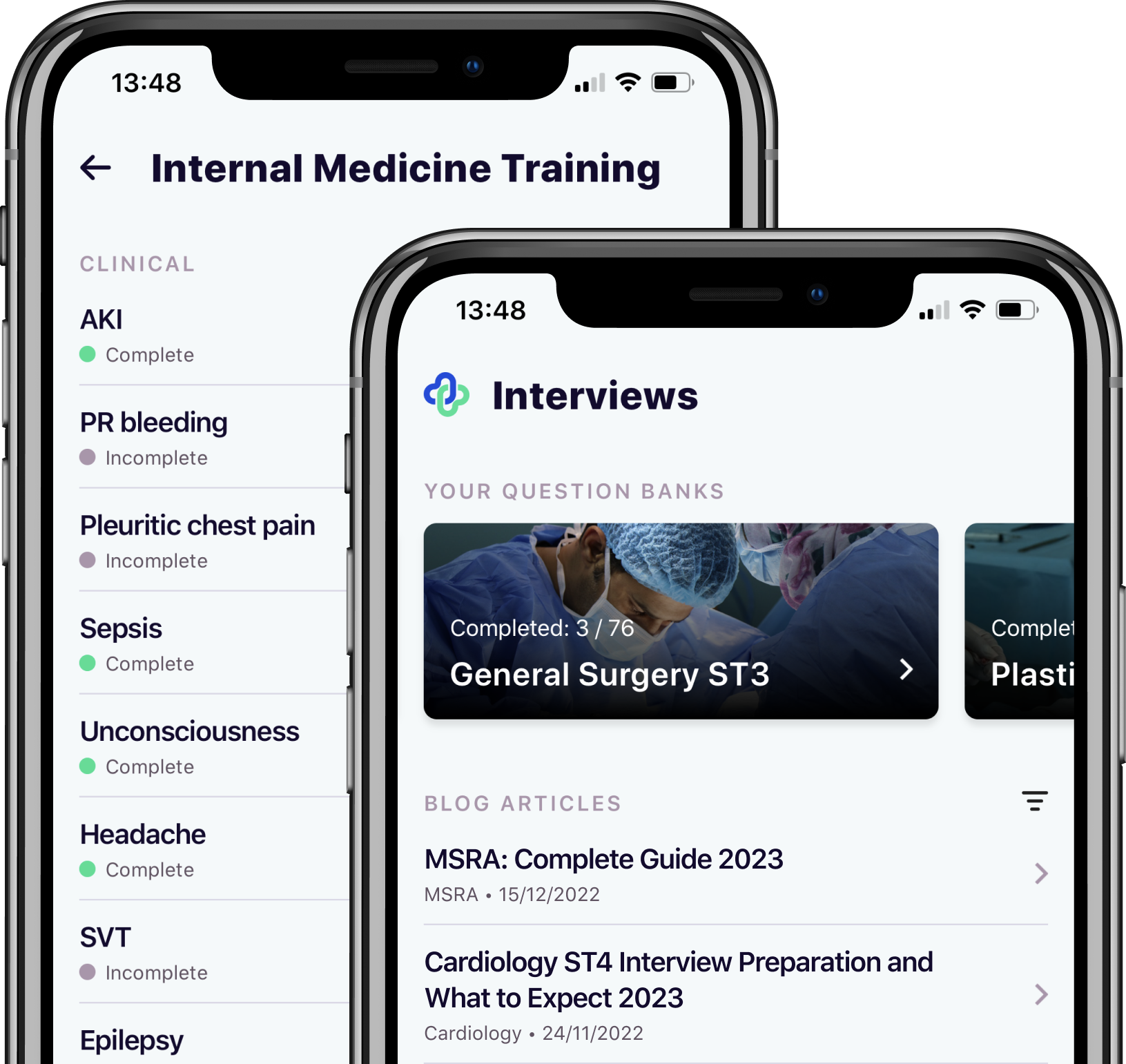
The Medibuddy adaptive MSRA question bank has been built with you in mind. Preparing for interviews and exams, working full-time and trying to maintain a work-life balance can be incredibly tough. We know, we have been through it ourselves!
Take your MSRA revision to the next level with our artificial intelligence powered, adaptive question bank
Our state of the art algorithms will help you progress faster than ever.
Our question bank has been designed using sophisticated AI-powered algorithms which help you prepare quickly and efficiently. Unlike regular question banks, our algorithms tailor learning specifically to you, as opposed to just giving you access to a huge database of questions. We won’t randomly give you questions; we will provide questions that will actually increase your exam score.
Practice is especially important in the clinical component and can also be useful in your interview. It is usually based on generic, GP-tailored medical knowledge, which is a useful refresher for some basic interview questions. Here is an example of a clinical question from our MSRA question bank.
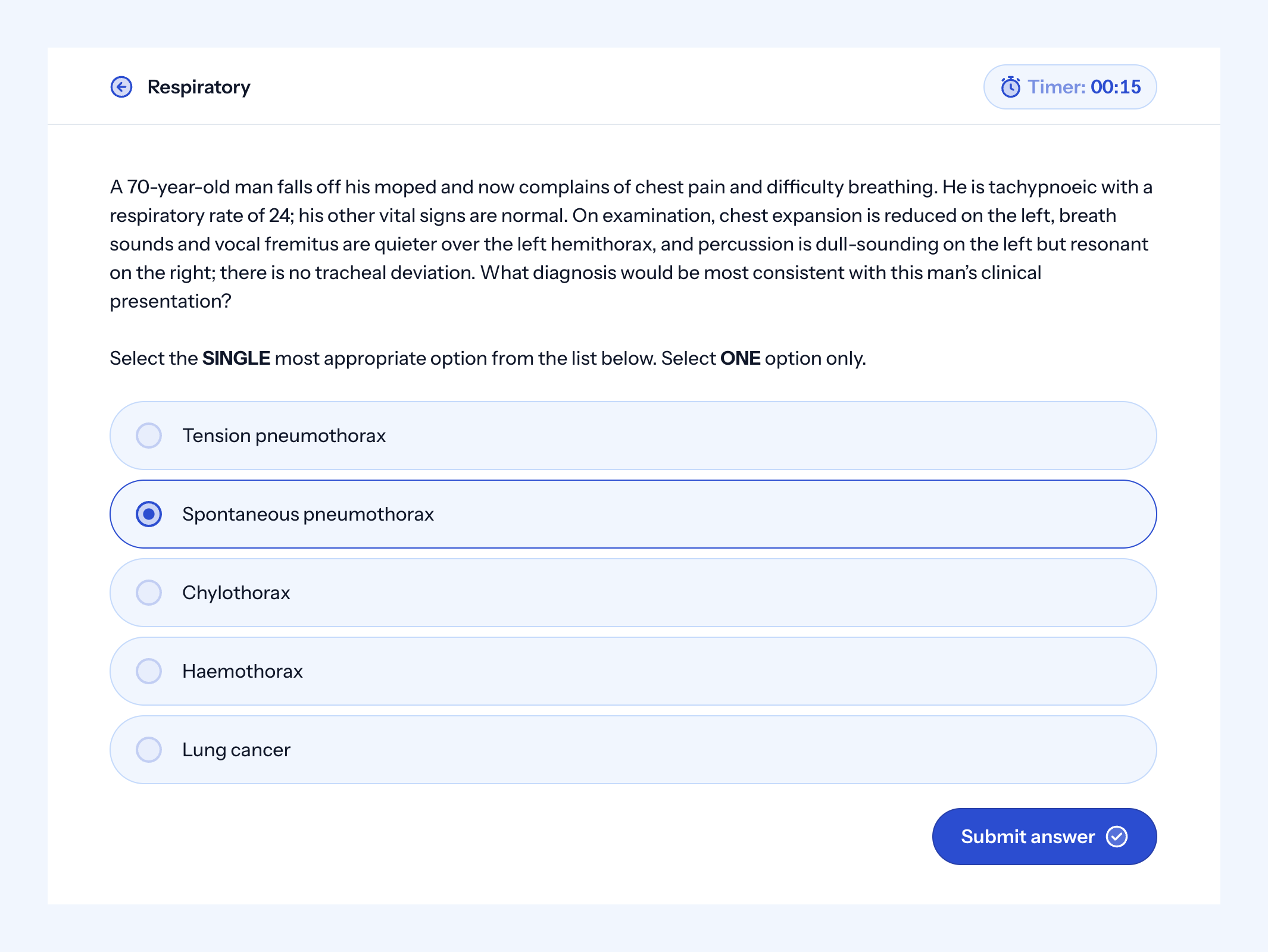
You can find out more about our question bank here.
Ophthalmology ST1 Interview Format
For 2024, the interview will have two components. This has changed from 2023, and we are currently updating our question bank to reflect this.
- Component 1: Assessment in the form of clinical knowledge
- Component 2: Assessment will be in the form of a medical consultation focusing on a difficult communication or ethical scenario
You will be invited to book your online interview if you meet the required MSRA score. Interviews are scheduled to take place between 2 January and 22 March 2024.
Ensure you have a strong wi-fi connection, a good laptop camera and room lighting, and are familiar with Microsoft Teams. Ensure that you have tested this prior to your interview!
Each component involves a patient consultation with an actor and will be up to 10 minutes in length, but be sure to give 30 minutes for your interview, including identity checks, the assessment and debrief. You will be tested on your clinical knowledge and communication skills. As with previous face-to-face interviews, clinical scenarios and communication skills tend to be fairly realistic and based on real-life scenarios as an ophthalmologist that you would encounter in your clinic.
There could potentially be a wide range of different topics based on various themes. As a suggestion, do prepare to be familiar with the following scenarios as a starting point:
- Patient with decreased vision, with diabetic retinopathy/maculopathy. You explain to them what the disease is, how it affects vision, treatment options, lifestyle advice and diabetic control.
- Patient with glaucoma, with progressing visual field loss and inadequate eye pressure control. You need to advise them about treatment compliance and disease progression, and always remember to check a social history, e.g. driving – do they meet the driving standards? What do they do for a living?
- Angry patient: common scenarios involve previous misdiagnoses (or poorly explained diagnoses), cancelled/delayed appointments and treatments not working.
- Refractive surprise: patient after cataract surgery noticing much worse vision – how would you approach this and what investigations would you instigate?
- Breaking bad news: for example, incidental finding of ocular metastasis. How would you begin a difficult consult like this? What does the patient know? What are your suggested next steps?
We have various example questions within our question bank, written by current ophthalmology trainees who ranked in the top 5% of the 2022 application cycle, and the picture below gives you a flavour of what to expect when you purchase.
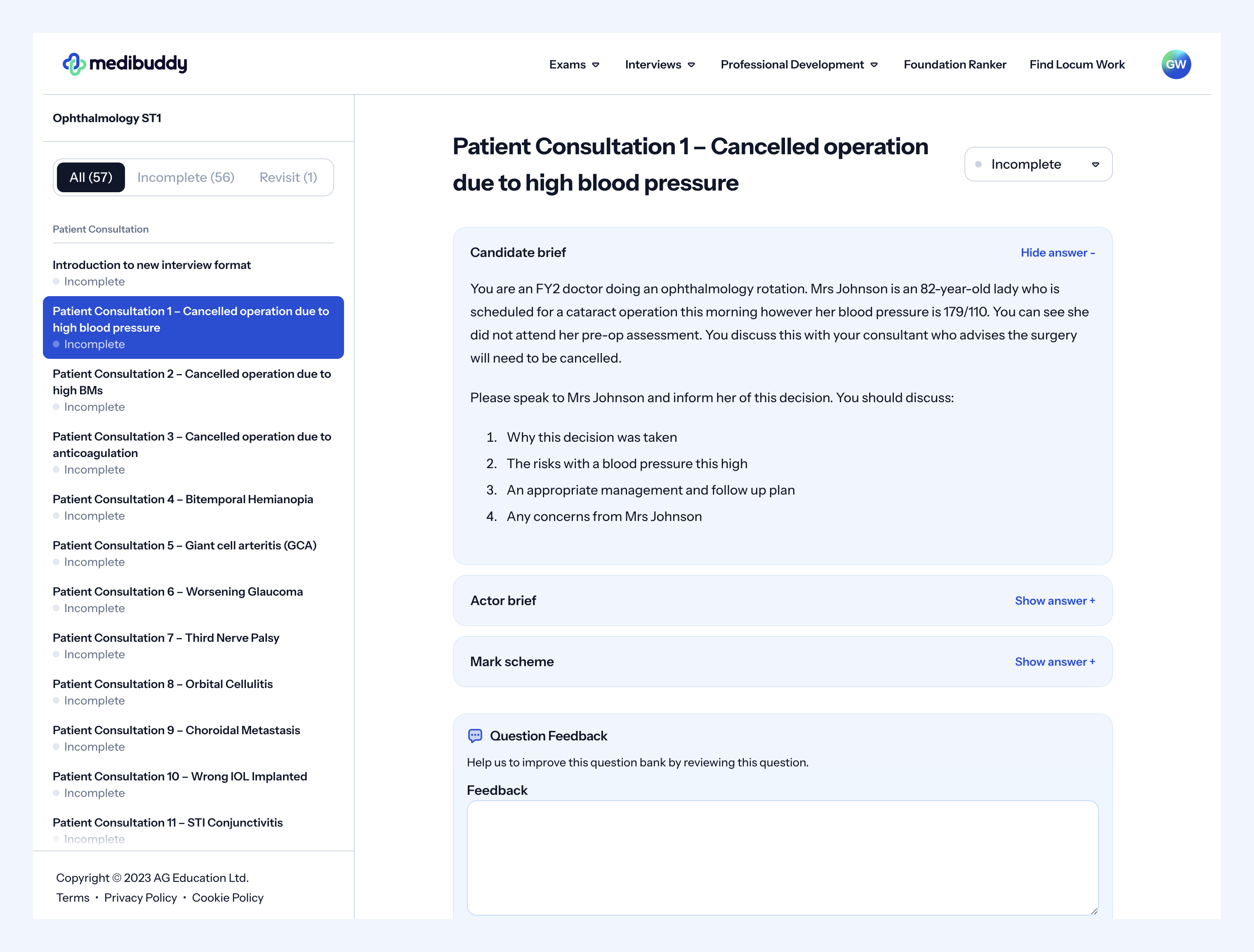
Although there are no specific QIPP/Audit stations this year, these are overlapping and very relevant themes in ophthalmology in general. Therefore, we have left these scenarios in our question bank for reference, and we recommend you read through these scenarios to familiarise yourself with cases like this and beyond. It is always easier if you have encountered real-life situations like this in a clinical setting, so do try to gain some prior ophthalmology clinical experience if you can. Use your taster week wisely!
Final tips
- Get started as early as you can! Get your evidence folder in order, as it takes a lot longer than you expect.
- Put time aside to practise for the MRSA exam and do lots of questions.
- Prepare for the online interview as you would with real-life OSCE stations. Practise with a partner online on Microsoft Teams for familiarity.
- Remember, you are scored stringently with a mark scheme, and almost half your battle is done when you submit your evidence folder.
- Coming across as well-mannered and thoughtful is always important at any interview and especially on a video call.
Good luck!
Take your subscriptions with you
Our mobile app allows you to access your interview and exam question banks wherever you are.