
How to Maximise Points in the 2025 Core Surgical Training (CST) Interview Portfolio
For 2025, Core Surgical Training (CST) interviews are being held between February to March 2025, which is slightly later than they were in 2024. There is a fairly quick turnaround from MSRA results and interview invites to the interview window, so we recommend being fully prepared where you can! Whether you are a foundation year doctor, medical student or taking a year out of training, if you are serious about applying for surgical training, it is important to understand how the portfolio section has changed to put yourself in the strongest position.
We will break down the Oriel Portfolio Scoring for 2025.
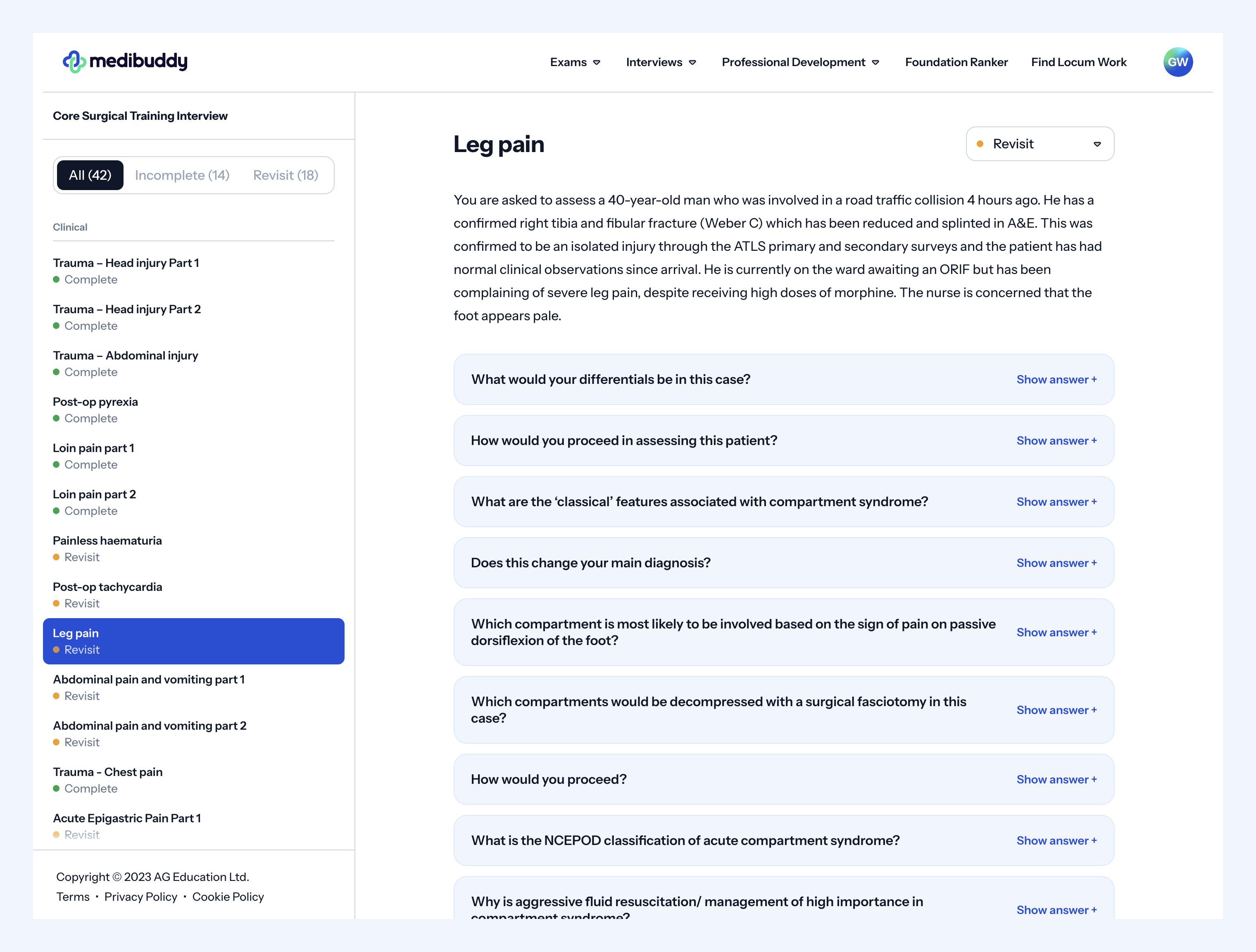
You can also check out our Core Surgical Training Interview Question Bank, which has been put together by previously high-scoring trainees to help you prepare for that all important interview.
2025 Core Surgical Training Interview
The MSRA continues to be used for shortlisting in 2025, with the 1200 top MSRA candidates being invited for interview. The 2025 MSRA exam is scheduled between Thursday 2 to Monday 13 January 2025, and the Core Surgery interviews will run between Monday 24 February to Friday 7 March 2025, with invites sent on Thursday 6th February 2025. This year, interviews will continue to take place online on a video platform called Qpercom. You will receive instructions on how to use this prior to your interview.
CST interviews will consist of one 30-minute interview divided into 3 x 10-minute stations, comprising a management station, a clinical station, and a portfolio station. These stations will be back to back and conducted by the same interview panel.
The domains for 2025 are as follows:
- Commitment to surgery
- Quality Improvement / Clinical Audit
- Presentations and Publications
- Teaching experience
CST Application points
For 2025, your CST portfolio is worth 30% of the overall score and assessed during the interview. This is different to previous years where the portfolio was assessed during the self-assessment part of the application process.
During the interview, assessors will have a 10-minute window to review the evidence you’ve uploaded as part of your portfolio. After this review, you’ll join them for a 10-minute discussion focused on two of your achievements. The assessors will select which achievements to ask about during their review, so be prepared to discuss any aspect of your portfolio in detail.
Your final portfolio score will be a combination of the assessor’s evaluation of your submitted evidence and your performance during the interview, based on how well you answer the questions about the selected achievements.
The remaining 70% comes from your MSRA score (10%) and the management and clinical stations (60%) With the majority of points coming from your interview, preparation is key and our Core Surgery Interview question bank will help. Here is an example of a clinical scenario from our interview question bank so you know what to expect. Our CST trainees have pulled together all of the themes of questions asked in the past years recruitment rounds, ensuring you have all of the tools to help you prepare for your interview.
The Core Surgery Training (CST) Portfolio
We have broken down each portfolio section to help guide you when putting your portfolio together.
Scoring for all domains has shifted from a numerical system to letter grades (A to E), with each grade requiring a specific level of supporting evidence.
Commitment to surgery
This is a broad section of the portfolio with points in various categories. Please note, this section no longer includes the MRCS Part A.
Operative Experience
Having at least 40 surgical cases assisting or supervisor trainer scrubbed is needed for the highest grade. This has continued to increase over the years, reflecting the competitive nature of CST. Keeping an eLogbook of surgical cases should begin at medical school and is useful for monitoring your progress through training. The summary sheet is required to be signed by a consultant.
| Option | Indicator | Notes |
|---|---|---|
| Operative experience: choose one of the following options | ||
| Involvement in 40 or more cases | A | Verified logbook evidence must be provided |
| Involvement in 30-39 cases | B | |
| Involvement in 20–29 cases | C | |
| Involvement in 11-19 cases | D | |
If you do not provide any evidence or have been involved in 10 cases or less, you’ll receive an E and won’t score any points.
Surgical Experience
Doing a surgical placement (with redeployment included) OR a surgical elective will get full points here.
If you are a student, it is recommended you complete a surgical elective, and then ensure you reflect on it for evidence. Although usually undertaken at medical school, you can also do short electives in your FY3 if applying then. Some bursaries are available from surgical societies if undertaken later, with potentially more opportunities for hands-on surgical experience.
If you have not had the opportunity to do a surgical placement, a 5 day taster week will get you the highest grade. Use this as an opportunity to try out a subspecialty of interest to help you with preferencing your surgical jobs in CST. You can also use it to increase your operating logbook, network with surgeons and sign up to research or audits.
| Option | Indicator | Notes |
|---|---|---|
| Surgical experience: choose one of the following options | ||
| I have attended a surgical taster week (minimum 5 days, can be non-consecutive days) | A | Proof of completion required |
| I have undertaken an elective in a surgical specialty (minimum 4 weeks), OR I have undertaken a surgical placement (see additional notes below) during my foundation training or equivalent (minimum 12 weeks) | A | |
| I have not attended a surgical taster/ elective | B | |
Quality Improvement (Clinical Audit)
This section focuses on demonstrating the complete process of a quality improvement project. You need to show your role in designing the project, collecting data, presenting findings, identifying areas for improvement, implementing change, and reassessing the outcomes.
Full marks in this section requires you to have “lead in ALL aspects of a surgically themed clinical audit or QI project that has demonstrated change” (i.e. second cycle/ closed audit loop). This should be achievable if you choose a project early (ideally FY1 year).
Notes:
For the 2024 selection process, changes have been made to the scoring of the Quality Improvement (QI) and Clinical Audit sections of the portfolio. Notably, presenting audit results at conferences and winning prizes no longer counts towards a higher grade, shifting the focus to the quality and impact of the project itself.
It’s still beneficial to engage in large, high-quality audits or QI projects that lead to measurable improvements in clinical practice. Projects that demonstrate real change continue to hold weight, even though higher grades for conference presentations or awards are no longer available.
| Option | Indicator | Notes |
|---|---|---|
| I was involved as Lead in ALL aspects of a surgically themed clinical audit or QI project that has demonstrated change (i.e., second cycle/closed audit loop). | A | You participated in all stages of the audit/QI project (planning, data collection, data analysis, implementing change and involvement in at least two cycles). The project must be surgically themed. |
| I was involved as Lead in ALL aspects of a clinical audit or QI project that has demonstrated change (i.e., second cycle/ closed audit loop). | B | You participated in all stages of the audit (planning, data collection, data analysis, implementing change and involvement in at least two cycles). |
| I was involved as a contributor in a clinical audit or QI project that has demonstrated change (i.e., second cycle/ closed audit loop). | C | You participated actively through multiple cycles but did not take a leading role in the project. |
| I was involved in a clinical audit or QI project. | D | For example, you assisted with data collection for the project in at least one cycle. You did not take a leading role. |
| None/other | E |
Additional points:
| Option | Indicator | Notes |
|---|---|---|
| Applicant presented both cycles of data or presented the intervention and change aspects of a project at a meeting | A | The applicant personally presented the project evidenced by first author in the presentation slides and letter of acceptance of presentation for meeting. |
| Applicant presented one cycle of the project at a meeting | B | The applicant personally presented the project evidenced by first author in the presentation slides and letter of acceptance of presentation for meeting. |
| Applicant did not present any aspect of the project | C | The applicant personally presented the project evidenced by first author in the presentation slides. |
Presentations and Publications
Planning ahead is essential when aiming to publish work or present at conferences, as these processes often take time. Original research can be challenging, but case reports or review articles may offer a more accessible path. Engaging with academic consultants can open doors to opportunities for publications and presentations.
Publications must be PubMed-cited, and chapters in medical books require an ISBN. Pay-to-present conferences do not count as peer-reviewed presentations. You may not gain a grade for the same audit as you gained a grade for in the Audit/ QI section. Instead, ensure you claim grades only for projects not used elsewhere in your portfolio, and select the option that awards you the most.
| Option | Indicator | Notes |
|---|---|---|
| I have won a prize for delivering an oral presentation at a national or international medical meeting convened by an accredited institution after being invited/selected to do so | A | Personal delivery of presentation required. This does not include “oral poster presentations” |
| I am first author (please see appendix for definition) of a PubMed-cited publication (or in press) not including a case report or editorial letter | A | Evidence of PubMed ID number. |
| I have delivered an oral presentation at a national or international medical meeting convened by an accredited institution after being invited/selected to do so | B | Personal delivery of presentation required. This does not include “oral poster presentations” |
| I am first author a prize-winning poster or oral poster presentations presented at an international or national medical meeting convened by an accredited institution after being invited/selected to do so | B | Personal delivery of presentation required. |
| I am first author of a PubMed-cited publication of a case report or editorial letter (or in press) OR I have written a book chapter related to medicine which has been published (not self-published) | B | Evidence of PubMed ID number. |
| I am a named co-author (please see appendix for definition) of one PubMed-cited publication (or in press) | C | |
| I am first author for a poster or oral poster presentations presented at an international or national medical meeting convened by an accredited institution after being invited/selected to do so | D | |
| I have given an oral presentation at a regional medical meeting after being invited/selected to do so | D | |
| I have given an oral presentation at a regional medical meeting after being invited/selected to do so | D | Personal delivery of presentation required |
| I have presented one or more posters as first author at a regional medical meeting(s) after being invited/selected to do so OR I have had a poster accepted for presentation at a national or international meeting but did not attend | D | Does not require oral presentation of work |
| I am a Cited Collaborative author as part of a research collaborative publication | D | Does not require named authorship alongside publication title |
| None/other | E |
Teaching Experience
Teaching experience offers a valuable way to enhance your Core Surgical Training application, even if medical education isn’t your primary career goal. Teaching opportunities could involve peers, medical students, or other healthcare professionals. To score the highest grade, candidates must organise and deliver at least four teaching sessions, which can be done individually or in collaboration with others.
Evidence is required, including letters from consultants confirming your involvement in designing and delivering the programme, along with formal feedback from participants or a senior observer, which must be verified but doesn’t need to be submitted directly. If in-person teaching is limited, virtual teaching sessions are a flexible alternative, and collaborating with your hospital’s education department can further boost your application.
You can also improve your teaching experience and boost your application by completing a course like the Medibuddy Teach the Teacher Course.
How to set up a teaching programme
-
-
-
- Start as early as possible, e.g. in induction week
- Briefly plan a program, e.g. session titles, audience, setting, teaching style, teachers, e.g. others colleagues/ junior doctors.
- Discuss the plan with your education supervisor during the first meeting as they may be able to assist.
- Discuss with the medical education department and arrange meetings with the head of medical education to discuss your proposal.
- If approved, you will need to plan the program in more detail
- Following this, the medical education department will usually email junior doctors asking for volunteers to prepare and deliver teaching based on your topics, offering certificates and formal feedback.
- Since COVID-19, there has been a proliferation of virtual teaching and webinar series in surgery which offer an opportunity for teaching programmes. This may be the most straightforward way to set up a program which is accessible at a regional and even national level.
Option Indicator Notes I have worked with local educators to design and organise a face-to-face teaching programme (a series of sessions defined as 4 or more) to enhance organised teaching for healthcare professionals or medical students. I have delivered at least 4 sessions of that teaching A You have shown the ability to identify a gap in the teaching provided and have worked with local educators to design, organise and deliver a regional teaching programme. As part of this process, you will have had input into the programme objectives and outline of sessions delivered. I have worked with local educators to design and organise a teaching programme (a series of sessions defined as 4 or more) to enhance organised teaching for healthcare professionals or medical students in an online format. I have delivered at least 4 sessions of that teaching B You have shown the ability to identify a gap in the teaching provided and have worked with local educators to design, organise and deliver a local teaching programme. As part of this process, you will have had input into the programme objectives and outline of sessions delivered. I have worked with local educators to design and organise a teaching programme (a series of sessions defined as 4 or more) to enhance organised teaching for healthcare professionals or medical students. I have delivered at least 4 sessions of that teaching C You have shown the ability to identify a gap in the teaching provided and have worked with local educators to design, organise and deliver a local teaching programme. As part of this process, you will have had input into the programme objectives and outline of sessions delivered I have provided regular teaching for healthcare professionals or medical students over the last year (4 or more sessions/year) OR I have undertaken some educational activity focused on learning to teach D Examples of teaching include but are not restricted to regular bedside or classroom teaching, acting as a mentor to a student, acting as a tutor or delivering teaching in a virtual learning environment. This would include any form of educational event focused on learning the skills of teaching – such as a training the trainers course online or otherwise 
Teach the Teacher Course by Medibuddy
This two-day CPD-accredited online course will earn you 12 CPD points on completion. It’s entirely flexible, so you can complete it in two days or multiple sessions over a longer period. On completion of the course, you’ll receive a certificate for your portfolio that is accredited for CCT, interviews and appraisals.
Find out moreEvidence
For each domain, ensure you look at what evidence is required (e.g. letters, audit presentation, etc.) early enough in the process to give yourself time to gather it. More information can be found here. You must have your portfolio completed and submitted by Wednesday 19 February 2025 at the very latest, so ensure you have all of the evidence you need well before then.
Further Reading
CST Interview Preparation and Essential reading
Core Surgery Interview Question Bank
Personal background
I am a registrar who previously worked in a top ranked rotation in London, which includes plastic surgery (my chosen specialty). I was not top ranked at medical school; in fact I was in the 8th decile academically on my foundation application. I was definitely daunted when I first reviewed the points required for CST and did not think I would be able to achieve enough points to obtain a job which included my chosen specialty, let alone in my chosen region. Please do not be put off by the points sheet and note that medical school academic performance is worth a minority of points on the interview application. The majority coming from other work in areas such as audits, teaching, clinical performance and projects work (presentations and publications).
I would suggest you read carefully the previous interview points specifications and set your own objectives on how you can achieve them. I would also recommend that you work with others, find mentors, form groups and share the workload involved in teaching, doing audits and research projects. There is a lot of work (and unfortunately expense) involved in scoring highly on the application and collaborating with peers makes this much more manageable. Please feel free to get in touch if you have any specific questions regarding the portfolio.
Mr Peter Macneal MBChB BSc PGDip (Clin Ed) MRCS (Eng)
-
-
Take your subscriptions with you
Our mobile app allows you to access your interview and exam question banks wherever you are.





