
Obs and Gynae ST1: A day in the Life of a Trainee
Hello, I’m a current Obstetrics and Gynaecology ST1 and I want to tell you about my training year, my average week and what I do day-to-day. As an ST1, we cover the junior rota alongside GPST2s and FY2s. Typically, in most hospitals, the ST1s will be given opportunities to cover more useful areas (the fun stuff) to develop our training. So I can cover; gynaecology emergency admissions, gynaecology theatre, maternity assessment unit, labour ward, elective C/sections, and ‘the day ward’ (observed TOP / MVA). I am less often asked to cover routine antenatal/postnatal wards compared to other doctors on the junior rota (you’ll still never fully avoid discharge letters!). I feel like every day is different and every day is interesting – there are hundreds of skills to conquer in O&G and each day I get to learn something new and work on developing independence in these skills.
A year as an Obstetrics and Gynaecology ST1
An amazing benefit of being an ST1 in a run-through programme is that your seniors are interested in helping you develop skills and will often find you when something exciting is happening to let you do it or to let you watch if it’s something you’ve not seen before. In a run-through programme such as O&G, all the doctors you work with will be your colleagues for the rest of your career, there’s no atmosphere of competition and everyone works to make sure you’re meeting your portfolio requirements. In stark contrast to being an FY, you get offered so many opportunities to send portfolio forms (several times per day) that I have a backlog of Mini-CEXs, OSATs and CBDs to send out to seniors for sign-off.
The RCOG oversees your training and you complete your portfolio through their trainee online portal. Currently, as an ST1, the bare minimum of technical skills to progress to ST2 is the ability to do cervical smears. Obviously, in a year you will want to do a lot more than that! I’m hoping to be signed off as ‘Entrusted to act under direct supervision’ in elective C/sections, non-rotational forceps, non-rotational kiwi and repair of 1st/2nd degree perineal tears by the end of the year. You are assigned an educational supervisor and will have a local college tutor to support your learning and development. Again, another amazing thing about being a trainee is that you are in one place for a year and have the same supervisor for a year. Your supervisor meets with you monthly (although you’ll probably see them more often than that on shift) to see how you’re doing, see what skills you’ve been working on, see what you still need help achieving and what clinics they can help you get into to support your learning. Your regional lead will email you frequently with learning opportunities, courses and teaching days to support your learning and portfolio. You get so many study days that we were told no one has managed to use them all in a year (I’m trying my best).
A typical week as an O&G ST1
Below is what I did this week – I’ll talk through some of the interesting things I did each day.
Monday: Maternity Assessment Unit 8:30 am-4:30pm
The maternity assessment unit at my hospital is a six-bed unit, alongside a 6-bed daycare unit (midwifery-led) and attached to the early pregnancy assessment unit (EPAS). Within the MAU I work very closely with midwives to look after any pregnant person unless they’d be better looked after by EPAS. So I most commonly see pathological presentations (i.e. things that aren’t supposed to happen in pregnancy) and the midwives manage presentations like; hyperemesis, at-term rupture of membranes, labour and first episode of reduced fetal movements.
Some of the interesting things I saw on Monday:
- A patient referred from ED with?PE in pregnancy (safe to go home on blood thinners and come back for a V/Q scan)
- Post-natal C/S wound infection (Needed to be admitted for IV antibiotics and a scan for ? collection)
- Bleeding in 2nd trimester (speculum didn’t indicate a cause, there were no signs of miscarriage, organised an ultrasound scan for assessment of placenta)
- At-term anti-partum haemorrhage (APH) that was stabilised and transferred to the labour ward for expedited delivery
- A non-specific presentation of lethargy post-natally that was a presentation of ‘baby blues’ (I spent lots of time with this patient to assess safety for them and the baby and get support in place for community follow-up)
Tuesday: Gynaecology Junior On-call 8:30am-8:30pm
On gynaecology on-call days, we begin in the labour ward by ‘huddling’ and finding out who is covering each role within the maternity hospital that day. I can swap bleep numbers with the obstetric junior and find out who the obstetric registrar is in case we need to cross-cover if we get busy. We then break off and get a gynaecology handover from the nightshift team to see what patients are on the ward, what beds we have available, who is waiting in ED to be assessed and which patients are waiting for a slot in the emergency theatre today. We went to the ward and completed the consultant-led ward round (9:00-11:00 am) then I began seeing emergency patients in our dedicated ‘gynaecology emergency unit’. These patients can come from the ED, be referred from the clinic, or come in from GPs.
Tuesday was a (quiet) day so I had lots of observed consultations and procedures for my portfolio:
- Saw a patient in very early pregnancy with lots of pain and reported bleeding. The speculum examination didn’t show anything concerning and I couldn’t see any bleeding. I’m not able to scan yet (TVUSS scanning courses are very overbooked just now and spaces often go to ST2/3/4s) so I asked my registrar to scan the patient. This showed a viable intra-uterine pregnancy (IUP) so all was well! Urine dip showed a significant UTI and the patient went home with their scan pictures and some antibiotics.
- Saw a patient from the post-menopausal bleed (PMB) clinic with low haemoglobin and heavy bleeding. They had known fibroids which had worsened and needed TXA and a blood transfusion. They were admitted for monitoring and planning for myomectomy as an in-patient.
- My last patient for the day was a woman admitted by the GP with abdominal distention, high Ca125 and pelvic mass on a scan who was not managing at home and needed admission for pain management, IV rehydration and further investigation.
At this time, CEPOD (emergency theatre) phoned to say our patient was next in line. We headed over to the theatre to meet the anaesthetists and scrub nurse team. My registrar and consultant allowed me to do my first surgical evacuation of the uterus for miscarriage with lots of support.
Wednesday: Postnatal Ward Cover 8:30am-4:30pm
Wednesday was an easier day – covering the postnatal wards. The midwives write a list of patients who need to be medically reviewed (most patients are midwifery-led discharges on the ward for uncomplicated births). I saw a few patients with larger than accepted blood losses – I assessed them for symptoms of anaemia and talked to them about iron replacement. I then saw a few patients who had been readmitted after discharge – one for endometritis, the other for a C/S wound cellulitis. I then completed any discharge letters for patients discharged on medications out of the midwifery formulary. In the afternoon, I floated down to the labour suite to see if I could do anything interesting and caught up on my portfolio.
Thursday: Elective Caesarean section list 8:30am-4:30pm
On Thursday, I was working with a great consultant who let me do lots of different bits of the elective C-Sections. I’m getting more and more confident as time goes on with different parts of the C-sections. I consented to the 5 women on the list and got to meet them and their birthing partners. We spoke about what was going to happen / what they were going to feel and what they wanted us to do when the baby was born. If the parents didn’t know the sex of the baby I offered the birthing partner a chance to stand up and see the baby. Three of the patients on the list were first-time mums so I completed the majority of their operations with the consultant watching and delivered my first breech baby by c-section. The two other patients on the list had more complex abdomens or a high risk of PPH so the consultant led those operations. We finished the last 30 minutes early so I sat with the consultant and they supported me in writing the operation notes.
Friday/Saturday/Sunday: Obstetric Junior Nightshift 8:30pm-8:30am
On the weekend I’m on the obstetric junior nightshift, which starts at 8:30pm and I leave the hospital at about 9am the next day. These are waking night shifts and I don’t get to nap at all! With the senior registrar, I cover the labour ward and the antenatal and postnatal wards. To start with, we hand over, go through the labour ward board and talk about high-risk births we might be getting involved in later. We then complete the evening ward round, introducing ourselves to the labouring patient, countersigning the CTGs and sometimes completing vaginal examinations to see how the patient is progressing in labour. After that, we go to see any high-risk patients on the antenatal ward who might come down to the labour ward through the night. From there – I run around answering bleeps for help with IV access, blood test result interpretation, high blood pressure and pain relief. At any time, my emergency pager can go off for me to return to the labour ward for emergency C-Sections. On my most recent set of obstetric night shifts; we did two emergency c-sections each night, I assisted with a forceps birth in theatre and we had a massive obstetric haemorrhage at 8 am on my last shift – this was the first time I’d seen a massive obstetric haemorrhage and the steps of emergency management we complete in theatre. Everything ran so smoothly during the emergency and the anaesthetist, registrar and charge midwife had such amazing communication that everyone in the room was aware of what we had tried and what was coming next.
The Training Pathway:
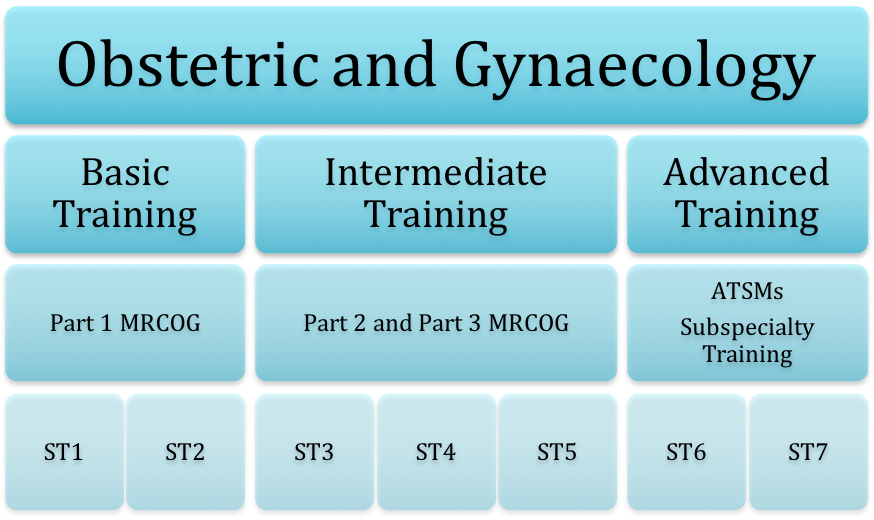
So coming next for me is to sit and pass MRCOG Part 1 and move into ST2. As an ST2, I will spend the first few months supernumerary, shadowing the registrar in both obstetrics and gynaecology and beginning to make senior decisions under direct supervision. Across the year, as I become more competent and confident I will meet with my supervisor to decide if they believe I can ‘step up’ into the senior rota and start working at a registrar level. The ARCP at the end of ST2 is when these decisions are formalised and personalised plans are put in place to support you as an ST3.
This blog was written by Suzie, an ST1 in NHS Glasgow and Greater Clyde.
Further Reading
Obs & Gynae ST1 Interview Preparation and Essential Reading
Take your subscriptions with you
Our mobile app allows you to access your interview and exam question banks wherever you are.





