
Obstetrics and Gynaecology ST1 Interview Preparation and Essential Reading
The key to acing the 2026 Obstetrics and Gynaecology ST1 interview is preparation. Candidates who spend time preparing and practising will be much more likely to score highly, as their answers will be slicker and they will be able to think more clearly under pressure.
This blog provides guidance on preparing for your Obstetrics and Gynaecology ST1 Interview, including useful links for further information. More detailed information about the interview can be found on our Obs & Gynae ST1 Interview Format page.
The ST1 recruitment process is run across the UK, so all the information will be provided by Health Education England, and the interviews are organised through the North West Local Office. All candidates, regardless of where they are currently training or where they want to work as a speciality trainee, will complete the same application and interview.
Essential Reading for Obs & Gynae ST1
The application process for Obs & Gynae ST1 is made up of the MSRA exam, and an interview. There is no longer a portfolio included.
There is some general reading that we recommend you do at the beginning of your interview preparation:
Overview of Applying to ST1 Obstetrics and Gynaecology
This website from Health Education England provides a very simple way to understand the different stages of the application process. It discusses this year’s recruitment timeline, how the Multi-Specialty Recruitment Assessment (MRSA) is used for Obstetrics and Gynaecology, the interview format and how you practically complete the application through the Oriel system. It also offers links to the different deaneries that offer ST1 training so you can start to think about where you want to work for the next seven years!
Personal Specification
The most up-to-date specifications for Obs and Gynae ST1 can be found on the Health Education England Website.
The person specification document includes the necessary entry criteria (things you must be able to show proof of) such as; having a medical degree, employment history, no fitness to practise concerns etc. But further into the document it also details the “desirable criteria” that are most likely to be assessed during the interview stage. This is when you need to begin considering how you can “evidence” your suitability for Obstetrics and Gynaecology. Take some time to read through each of the selection criteria and write down some bullet points of a time you have demonstrated your skills in each area.
Appointability
You need to score at least 50% in the online interview, and examiners need to have no concerns regarding patient safety during the clinical prioritisation section of the interview (regardless of overall score) to be able to deem you appointable. There are only a small number of candidates each year who are told they are unappointable, and being unappointable one year does not mean you cannot re-apply the following year. Scenarios that may cause you to be unappointable include; unprofessional behaviour during the interview section (swearing, ethical lapses etc.) or significant failure to recognise the severity of illness in the clinical prioritisation portion of the interview.
How Competitive is Obs & Gynae ST1?
For 2025 entry, there were 4945 applicants for 297 posts, meaning 16 people applied for each post. This is a big increase from 2024, when there were 2170 applicants for 310 posts, resulting in 7 people applying for each post. This indicates that Obstetrics and Gynaecology is a competitive speciality and is becoming more competitive as the years go on. Consider also that you don’t only want to be in the top 25% of applicants, but to get a training post where you want to live and work – you need to be aiming as high as you can. You can view post offers and acceptance rates here. The Health Education England website provides up-to-date and historical information on competition ratios for all specialities.
Multi-Specialty Recruitment Assessment (MSRA)
Everyone applying to Obstetrics and Gynaecology ST1 will take the MSRA exam, which makes up 33.33% of your final score. The 75 highest-scoring Obstetrics and Gynaecology applicants have the amazing opportunity to ‘bypass’ the interviews (i.e. not have to do them at all). Last year, the 75 applicants who bypassed the interviews were the top 1.52% of all 4945 applicants, so don’t pin all your hopes on bypassing, and continue to prepare for your interviews until you get the good news. However, considering the opportunity this presents and its importance to your final score if you do interview, it is essential that you prepare well for the exam.
Our MSRA question bank dashboard (below) shows a full list of the topics that you’ll be assessed on within the exam:
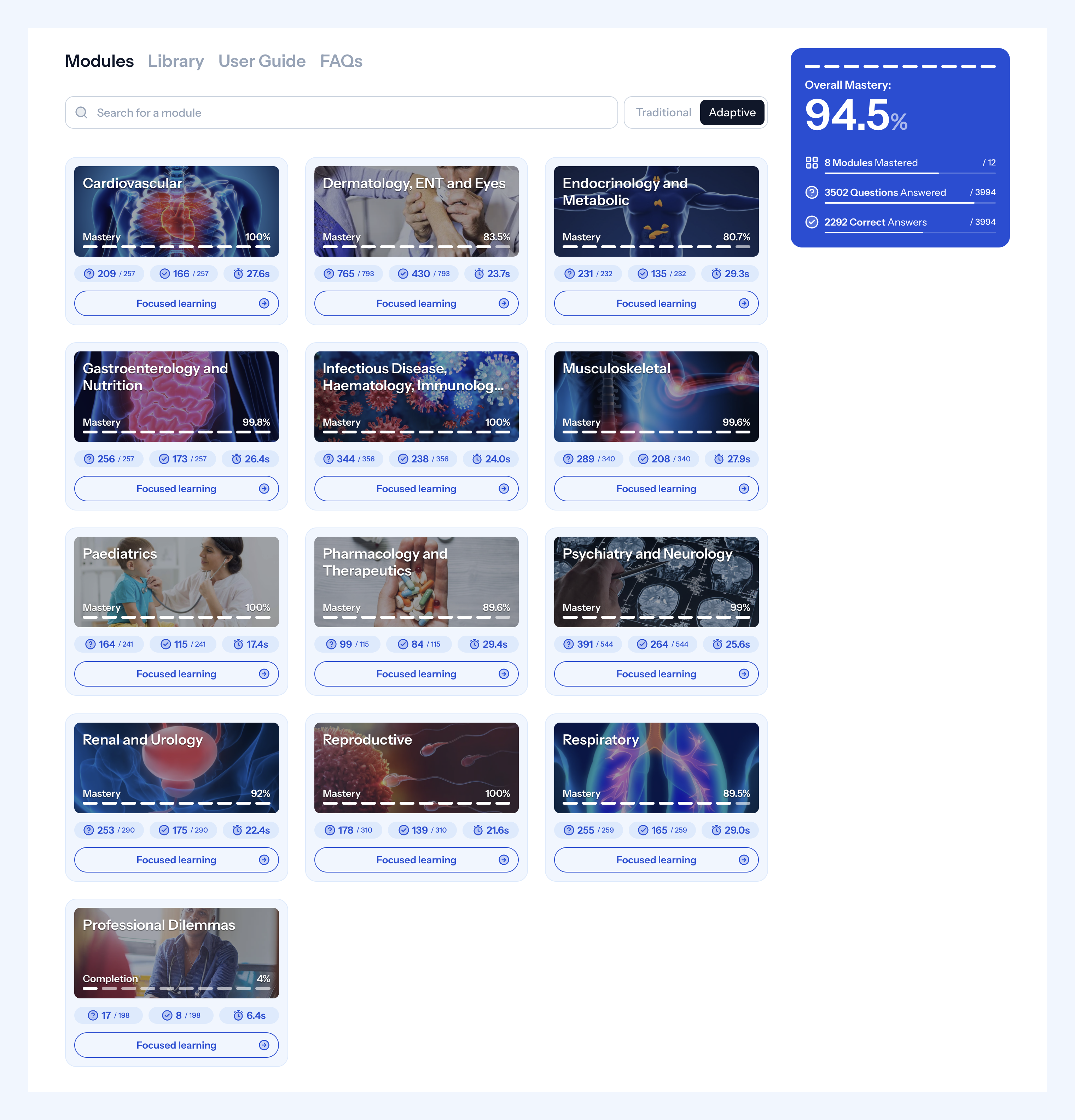
Medibuddy MSRA Question Bank Dashboard
To learn more about the MSRA format and how you’ll be assessed, visit our MSRA 2026 Complete Guide.
Your MSRA personal exam score is scaled from 0-50 of all applicants to obstetrics and gynaecology, this is then added to a maximum of 100 marks from the interview stage. Most applicants start preparing for the MSRA months in advance; we’d recommend you do the same and try to practise as much as possible before the exam. The Medibuddy Exam Question Bank is here to help! With over 4000 practice questions to help you make effective use of your MSRA revision time.
Take your MSRA revision to the next level with our artificial intelligence powered, adaptive question bank
Our state of the art algorithms will help you progress faster than ever.
You will be invited to apply and will receive lots of explanations about how to apply once the application window closes on Oriel. If you are applying to more than one speciality that uses the MSRA, you will only have to sit it once. More information about its use and scoring can be found here.
Obs & Gynae ST1 Interview
The Medibuddy interview format blog discussed the interview itself, including the three different questions; clinical prioritisation, ethical and governance, and the structured interview.
The Clinical Prioritisation and Structured Interview sections each carry 40 marks, while the new ethical and governance question replaced the communication question, and contributes around 20 marks to your overall interview score. This section is designed to assess your understanding of ethical and governance issues in a specific medical-related situation, a key requirement for anyone entering Obstetrics and Gynaecology.
Although the 2026 guidance provides limited detail on the interview format, the overall structure is similar to previous years. We’ve therefore included information on the Clinical Prioritisation and Structured Interview sections below to give you a clear idea of the types of scenarios and questions you’re likely to encounter.
The O&G ST1 interviews place online through Microsoft Teams or Qpercom software. Get comfortable with the equipment you’re going to be using during the interview, test your webcam and microphone and consider having a backup device. Make sure you have a quiet space to complete the interview and let everyone in your house know you need 30 minutes without interruption. I felt like being in my own space was more relaxing but concerns about technology leading up to the interview can cause some anxiety.
You can feel a disconnect between yourself and the interviewers due to the barrier of technology. Eye contact is trickier (do I look at the webcam or the interviewers on the screen?), and the slight delays in speech can make it seem like you’re talking over one another. I looked at the screen whilst the interviewers were talking, still using all the non-verbal communication skills we’re used to, then looked at the camera while speaking. Additionally, allowing a small gap between the interviewers finishing their questions and you starting to answer can prevent you from speaking over them. It can be uncomfortable to see yourself answering questions on the big screen – avoid looking at your own window during the interview, it gives the appearance of uneasiness if your eyes are darting about. The in-the-moment self-consciousness or judgement won’t help either.
However, in the lead-up to the interview, a great way to practise is by recording yourself answering questions, such as those provided in the Medibuddy question bank, and watching your performance back. You can see how you come across and see if there is anything you need to improve. Remember, it isn’t just what you say, it’s how you say it. I would strongly recommend practising with a trusted friend or colleague through a Teams call to get used to the online interview format. Record a whole meeting and watch it back to see if you’re happy with your interpersonal skills, if you’re engaged and smiling appropriately and if your voice is clear through the filter of technology.
The Obstetrics and Gynaecology ST1 application process used to include a portfolio station, similar to that of CST and Radiology applications. This was removed a few years ago, but some resources or books still talk about how you present your portfolio – don’t get confused by this. Although the formal portfolio was removed, it is still useful to collate your achievements, projects, presentations, course certificates and teaching evidence as if you were submitting a portfolio. After the MSRA is over, you can sit and look through everything you’ve done during medical school and foundation years – is there an audit that was especially good or presented at a high level? Did you forget about a teaching session you did that was gynaecology-specific? I found my portfolio folder a very useful prompt while preparing my interview answers.
Hints and Tips for the Clinical Prioritisation Station
This is the portion of the interview people are often more concerned about and put more preparation time into. There is no need to worry about this station, it is assessing your ability as a doctor at an FY2 level. Some of the cases may have some obstetric and gynaecology conditions but nothing an FY2 wouldn’t be able to handle. Think of this station as a verbal OSCE, what would you do if the patient was in front of you?
When the interview begins, you will have 5 minutes to read a set of scenarios including descriptions of 4 patients +/- NOK who need your assessment and care. Have a practised and rehearsed way of documenting this information – you are allowed a pen and paper. Take a moment to prioritise the cases. Typically one will be acutely unwell and one is a non-clinical matter (talking to next of kin, breaking bad news etc.) then slot the other two cases appropriately in the middle. Practice documenting the information a few different ways and find what works best for you.
I wrote the patient information down from what I assessed to be ‘priority patient one’ to ‘priority patient four.’ With space in between each case to then go back and document:
- Concerns/problems
- Initial actions (ABCDE)
- Who else can help
- Differentials
- Definitive management.
Once the 5 minutes of reading time is up, you will be given approximately 6 minutes to discuss your thoughts and action plan with minimal prompting or questions. The six minutes go by very quickly so practice makes perfect to ensure you are slick and confident in your answers. Begin by explaining your prioritisation and how you are going to format your answer.
For example: “Considering the availability of other colleagues, I would prioritise patient A (desaturation) as most unwell, followed by Patient B (temperature), Patient C (confusion) and lastly the non-clinically urgent, but important discussion with Patient D regarding a new diagnosis of malignancy. I will talk through my management for each patient in turn.”
Practising will help you avoid “jumping about” from patient to patient leading to confusion between yourself and the interviewers.
In terms of the content of the clinical prioritisation station; I had come across all the cases I was presented with in my clinical work many many times. The difficulty in this station is not the academics of patient diagnosis and management – it’s your ability to prioritise, delegate and communicate. A consultant (the interviewers) knows that an FY2 can recognise and manage sepsis – but in 90 seconds can you discuss the full management of sepsis, consider the source, delegate to an FY1 to take bloods/cultures/request scans and consider the need to escalate to level 2 care?
I found the Medibuddy clinical scenarios very helpful to practise with, they allowed me to consider all of the most common patient presentations; sepsis, MI, PE, post-operative complications, GI bleeds, stroke etc. They also covered the most common emergency Obstetric and Gynaecology presentations such as ectopic pregnancy, major haemorrhage, endometritis etc. Lastly, there are some good prompts for non-clinical scenarios that can come up such as the consideration of confidentiality, breaking bad news, recognition of errors in patient care, and interpersonal conflicts. I have included an example of a clinical prioritisation scenario below.
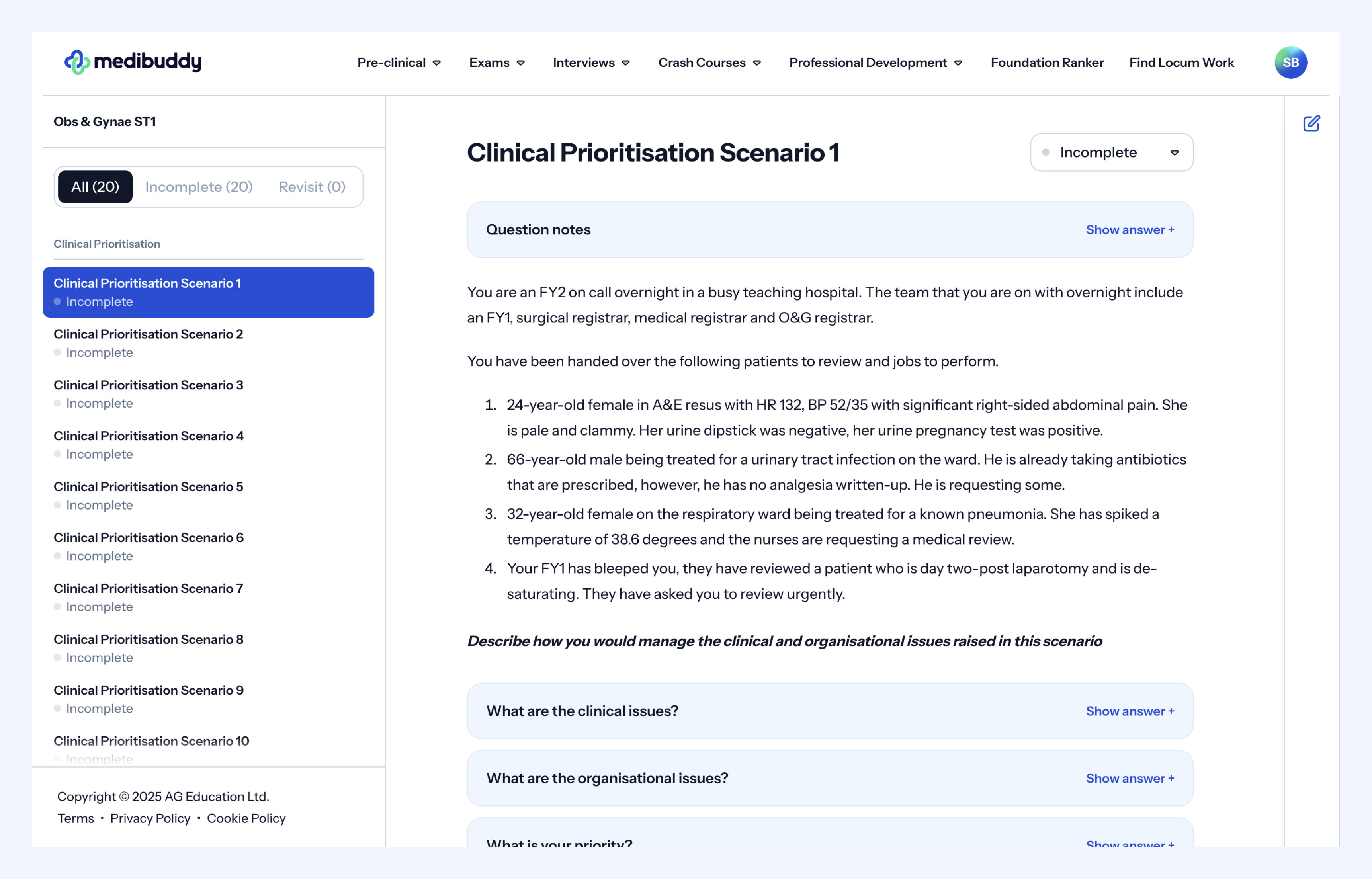
After you’ve worked through the clinical scenarios a few times you may be lulled into a false sense of security, “Well I know how to treat a blood transfusion reaction.” It is important to stress that this station is not only assessing your knowledge but your ability to communicate it under pressure. Always practise these questions out loud, and practice documenting the patient information within a time limit.
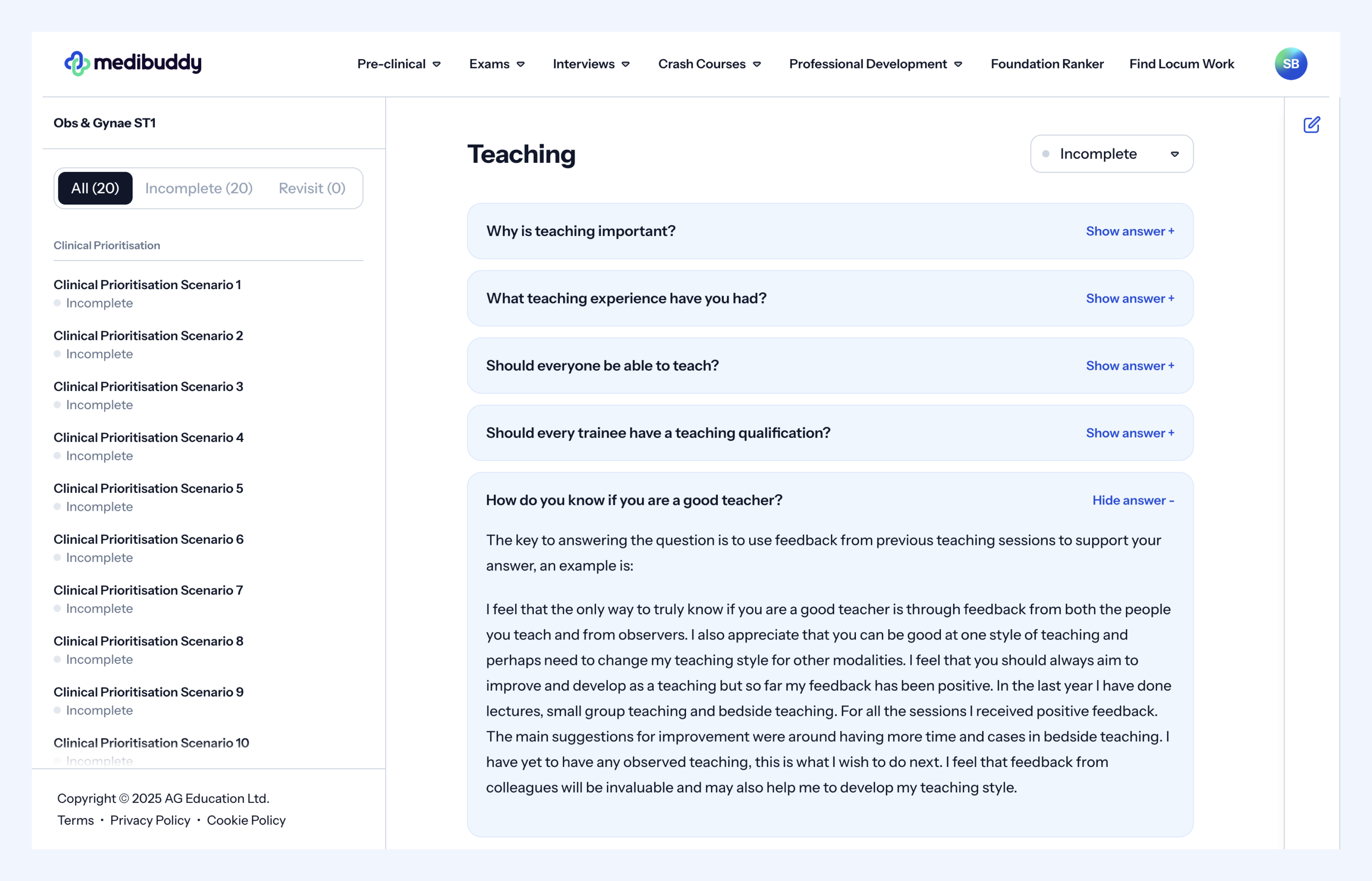
Hints and Tips for the Structured Interview Station
The structured interview station lasts approximately 9 minutes. There will be two interviewers who will ask you questions and one panel member who won’t speak. This station involved a very quick-fire set of questions that you must be ready to answer. There is limited time to pause and think so having several weeks of practice behind you will allow you to keep the pace of the interview. Due to the short amount of time and the volume of questions the interviewers have to get through, it can feel like they are cutting you off or not reacting to what you are saying – don’t let this rattle you. If the interviewers move on to the next question, they are likely happy with what you have said and want to hear your answer to the next question which may be assessing a different key attribute.
The structured interview station includes core topics:
- Commitment to the speciality
- Quality improvement measures
- Research and teaching
- Experience outside of medicine, leadership and teamwork
Questions will not only focus on what you have done but also on what you have learned from your experiences. Use this station to outline to the examiners your key selling points, your positive attributes and why they should employ you. Don’t answer a question by listing off all the things you’ve done – Consider reflection at each step:
- How did that audit help me develop as a clinician?
- Why was my taster week so beneficial in helping me decide to pursue Obstetrics and Gynaecology?
- Why was the teaching I did important to my role as a doctor?
I found the Medibuddy question bank very useful in helping me consider the niche aspects of questioning I wouldn’t have considered on my own, I have included an example of a structure interview question in the image below. Additionally, there will be questions not specific to yourself as a doctor. Each ‘topic’ was often rounded off with a more generalised question regarding the importance of the key attribute.
For instance:
- What is the difference between a QIP and an Audit?
- Should all doctors be teachers?
When considering “commitment to speciality” utilise experiences you’ve had within the speciality to answer the questions. If you’ve done an FY2 rotation, been a clinical fellow for a year or had a taster week – explain why this made you want to be an O&G trainee. The answer to “Why obstetrics and gynaecology?” will be different for everyone; but you know the question is coming so make it brief, make it slick, and make it sound great as your first soundbite to kick off the interview.
If you can talk about a personalised experience you’ve had this can project a very genuine decision – “During my FY2 rotation, I was drawn to not only the complex surgeries but also the psychological support women needed during the investigation of chronic pelvic pain. Historically I know the problems women have had when presenting with undefined pain and I want to be part of a speciality that supports these patients.”
Spend a significant amount of time on the RCOG website to ensure you have a detailed understanding of the O&G training pathway and curriculum. How many years long is training? When can you sub-specialise? What is an ASTM? What portfolio requirements will you have as an ST1? When do you have to sit MRCOG?
It is also important to have a realistic understanding of the speciality. It comes across as a more carefully thought-out and motivated decision if you can reflect on the less fantastic parts of being an Obstetrics and Gynaecology trainee. Consider what you’re least looking forward to about being a trainee and how you might get support for this. Consider the negatives of Obstetrics and Gynaecology as a speciality; high rates of litigation, high rates of trainee drop-outs, the emotional impact of maternal/ fetal deaths, several significant recent publications about poor care in women’s health departments, steady increase in the complexity of births, national midwifery staff shortages, reduced theatre opportunities in gynaecology so harder to gain competency before CCT. Reflect on these problems and be honest that you might not know how to deal with them now, but you’ll seek guidance and support from your seniors and supervisors.
How long should I take to prepare?
This fully depends on your learning style and which aspects of the interview you might struggle with. It is up to you how many weeks you designate for each stage below:
Stage One: Start gathering information after you have sat the MSRA in January. Make sure you understand the format of the interview. Start purchasing question banks to help you practise. Save/ print important information from the RCOG website about training. Read the MBRRACE-UK report.
Stage Two A: Start writing answers to each question you may be asked – remembering that you do not get a lot of time per question so no paragraph answers. Try to avoid attempting to memorise your answers, this can cause you to falter under pressure if you forget exactly what you wanted to say. Sticking to bullet points which you can comfortably expand upon will take the onus off of perfectly reciting an answer.
Stage Two B: Remind yourself of all the common clinical scenarios you may be asked about and how these are managed. If you’ve not had a rotation in O&G take some time reading about ectopics, PMB, endometritis, major haemorrhage etc. and the initial emergency management of these conditions.
Stage Three: Practice, practice, practice. Practise with family, practice with friends, practice on Teams. Find an ST1 or ST2 who can help you – they have most recently, successfully been through this and can give you the most up-to-date help. Avoid practising with your best friend or mum unless you’re sure they will give you honest feedback. Record yourself practising (I know it’s uncomfortable to watch but it will help!).
We hope you have found this blog useful and wish you the best of luck with your application.
Further Information
OG ST1 – Day in the life of a trainee
OG ST1 Interview Question Bank
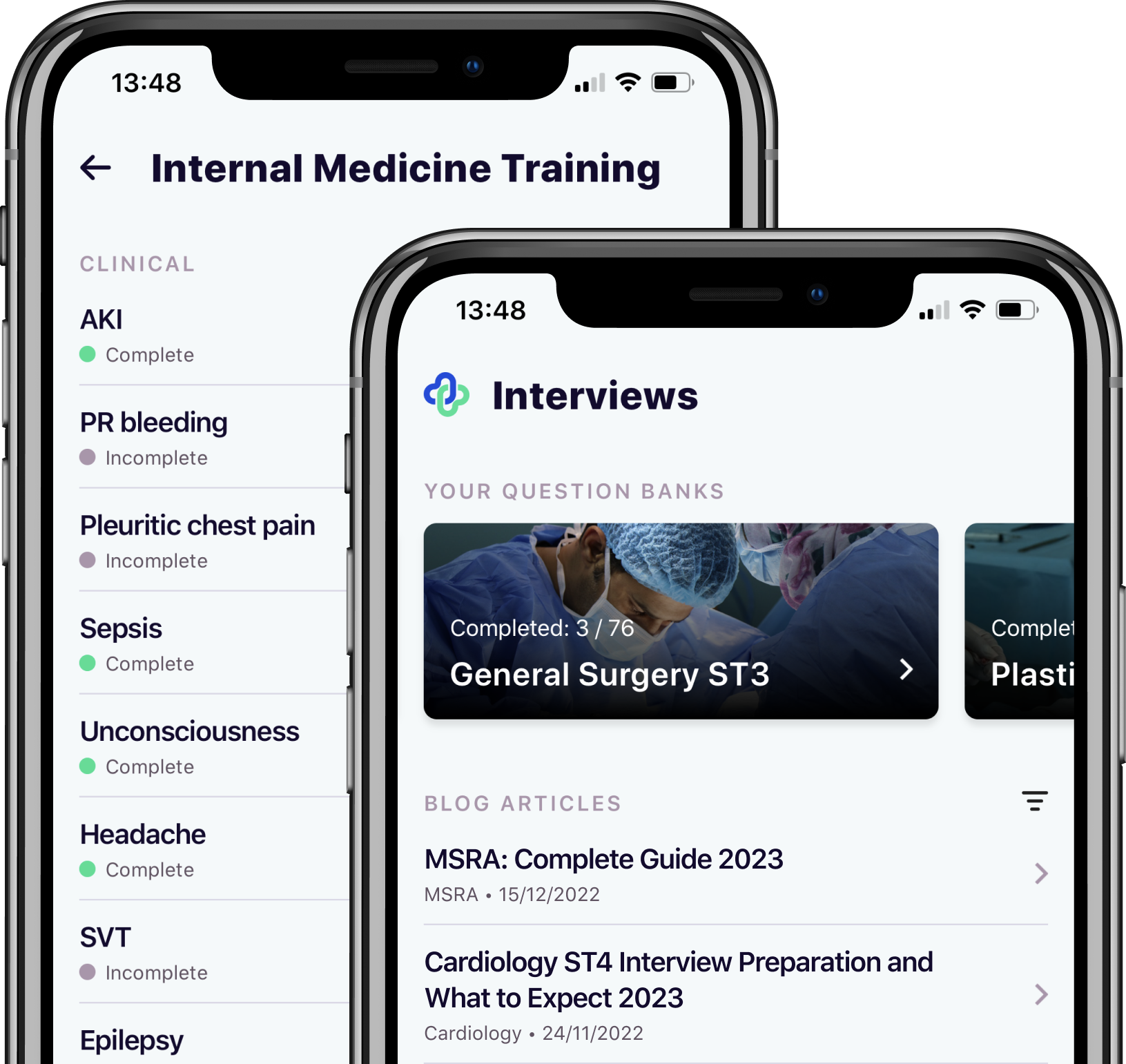
Take your subscriptions with you
Our mobile app allows you to access your interview and exam question banks wherever you are.





